
In today’s healthcare landscape, building a resilient, sustainable physician workforce has become a top strategic priority. Healthcare leaders recognize physician talent is one of their most valuable assets—essential to quality care, patient access, and organizational performance. Yet many are struggling to move the needle on physician engagement and retention despite significant investments and genuine efforts.
The challenge isn't a lack of commitment from leadership. Rather, a subtle disconnect has emerged between healthcare executives and physicians. This misalignment, even when unintentional, erodes trust—and the downstream impacts are serious: decreased engagement, higher turnover, reduced care quality, increased recruitment costs, and diminished patient access.
Discovering the root causes of physician disengagement
The goal of the 2025 Physician Sentiment Survey was to help healthcare organizations understand the engagement gap from the physician's perspective. In May of 2025, CHG Healthcare and Hanover Research surveyed 920 currently practicing U.S. physicians to uncover the root causes of disengagement and, more importantly, to identify the specific, actionable strategies that healthcare leaders can deploy to strengthen physician engagement and retention.
The report’s findings reveal that some of the most impactful changes are well within leadership control and don't require major structural overhauls or significant capital investment.
Read the executive summary:
Building a more engaged physician workforce
Although 75% of physicians reported being satisfied with their current role, only 18% were highly engaged in their workplaces. This satisfaction-engagement gap points to untapped potential and hidden vulnerabilities. While factors like compensation and autonomy ranked highest in physician priorities, these were often constrained by broader market forces. However, transparent leadership and open communication—which physicians also say they value highly—are entirely within leadership's sphere of influence and present immediate opportunities for meaningful improvement.
This report identifies where healthcare leaders can make the greatest impact, offering a clear roadmap for strengthening the physician-leadership relationship and building a more engaged, stable workforce.
Physician satisfaction and retention
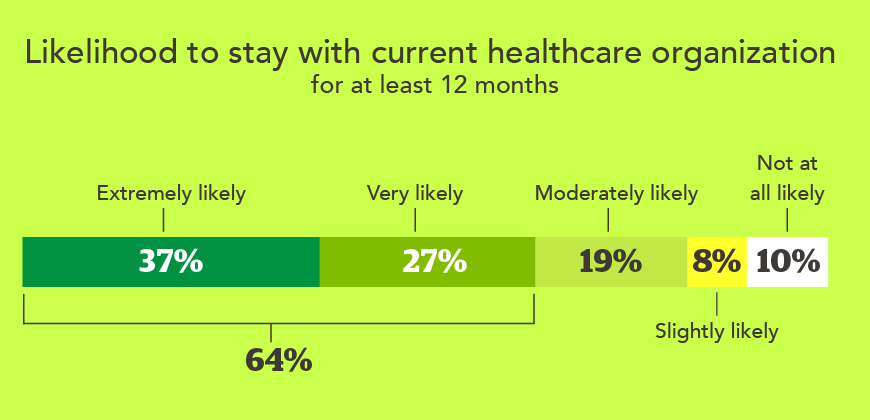
Overall, 75% of physicians say they are “somewhat” or “very” satisfied with their current role. This satisfaction translates into a strong likelihood that these physicians will stay with their current employer for at least 12 months. A total of 64% say they are “extremely” or “very” likely to stay.

Although many physicians report being at least somewhat satisfied and intend to stay, few are highly enthusiastic advocates for their healthcare organizations. Only 29% of physicians say they are likely to recommend their healthcare organization as a great place to work. Unfortunately, even more physicians (37%) say they are unlikely to recommend their organization, translating to an overall net promoter score (NPS) of -8.
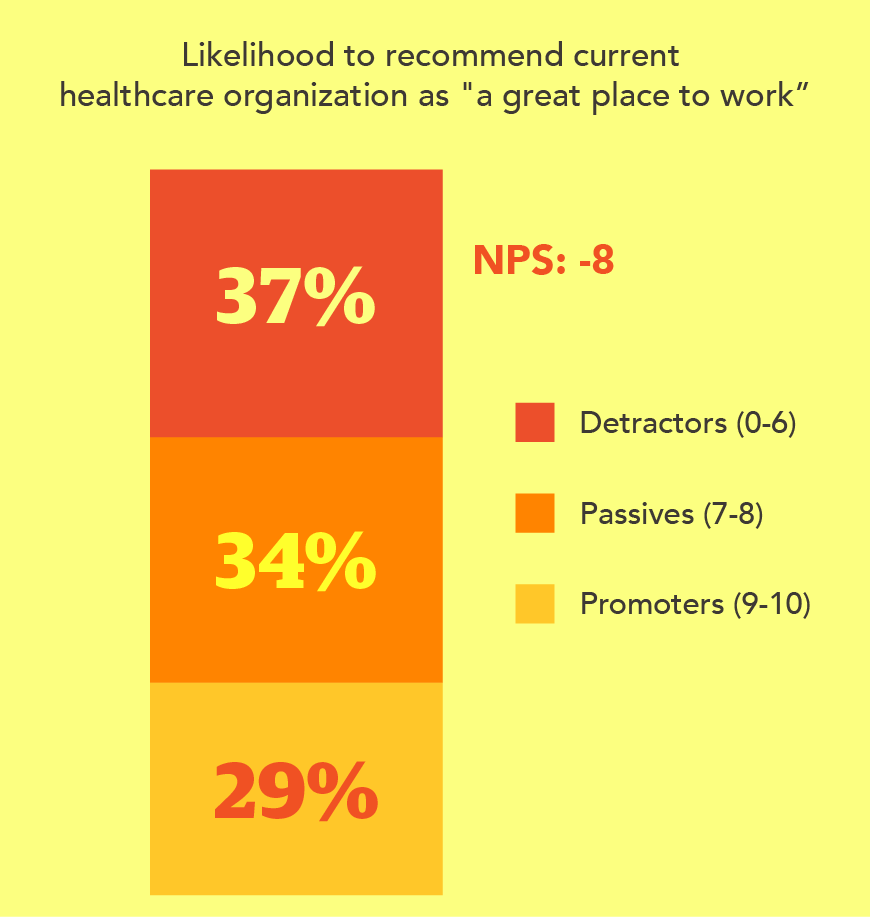
A negative net promoter score suggests that physicians are experiencing pain points not captured in their reported satisfaction level and raises red flags for recruiting efforts, referral-based hiring, and the prospects for long-term retention.
This satisfaction-engagement gap reveals a critical insight for healthcare leaders: Physicians may not be unhappy enough to leave immediately, but they're also not engaged enough to thrive, advocate, or commit long-term. The difference between satisfied and highly engaged physicians often comes down to their relationship with leadership and their voice in organizational decisions—factors that leaders can directly influence.
What makes a highly engaged physician—according to our research?
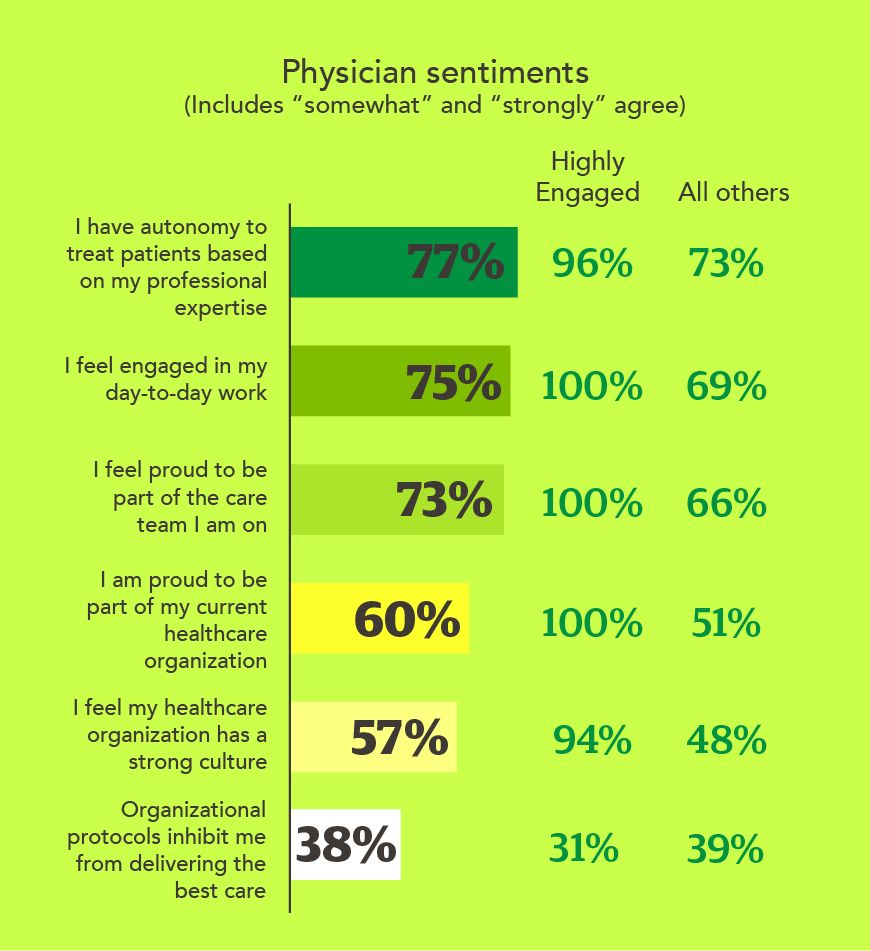
Survey respondents were segmented into two categories: “highly engaged” and “all others” based on four key indicators of engagement (see table below). The respondents who met all criteria comprised the “highly engaged” group, which totaled 18% (n=167) of the survey cohort.
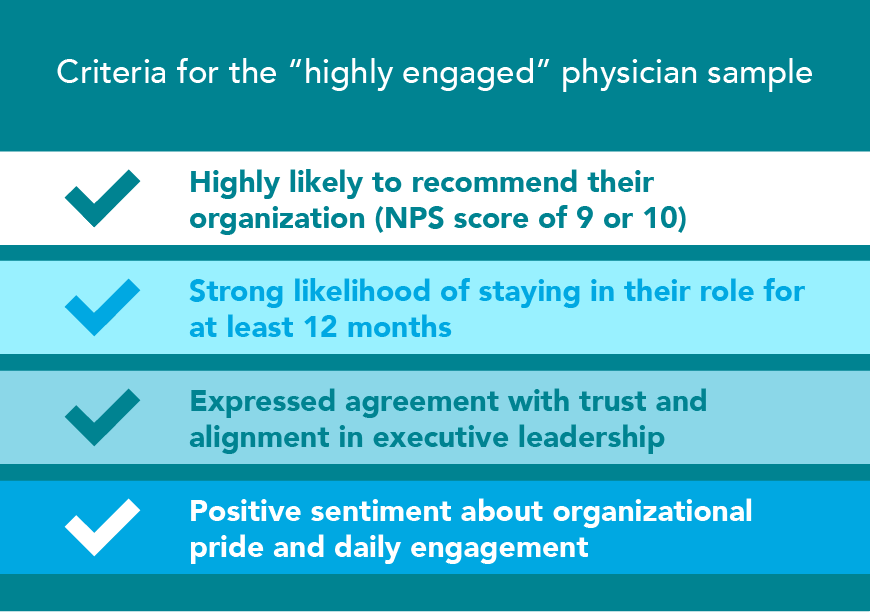
This segmentation allows a comparison between highly engaged and all other physicians, highlighting critical gaps in engagement, advocacy, and fulfillment. Highly engaged physicians demonstrated strong positive sentiments across a variety of topics, from feelings of autonomy to organizational pride and day-to-day engagement—all indicating a vibrant culture.
Physician workplace attributes: Importance vs. satisfaction
Physicians were asked to rate the importance of various aspects of their jobs and then rate how satisfied they were with those aspects in their current role. Gaps between importance and satisfaction highlight areas where healthcare leaders have the clearest path to effect meaningful changes.
While compensation and autonomy consistently top physicians' priority lists, these factors are often constrained by market forces, insurance reimbursement structures, and organizational financial realities. However, leadership transparency and communication—which rank nearly as high in importance—are entirely within leaders' control and can be improved immediately without capital investment or policy overhauls.
Compared to their less engaged peers, highly engaged physicians were 46 percentage points more likely to report satisfaction with leadership transparency, and 40 percentage points more likely to feel leadership communicates openly. These gaps highlight areas where leadership can make meaningful improvements through enhanced communication and transparency, without requiring major structural changes such as adjustments to compensation or work-life policies.
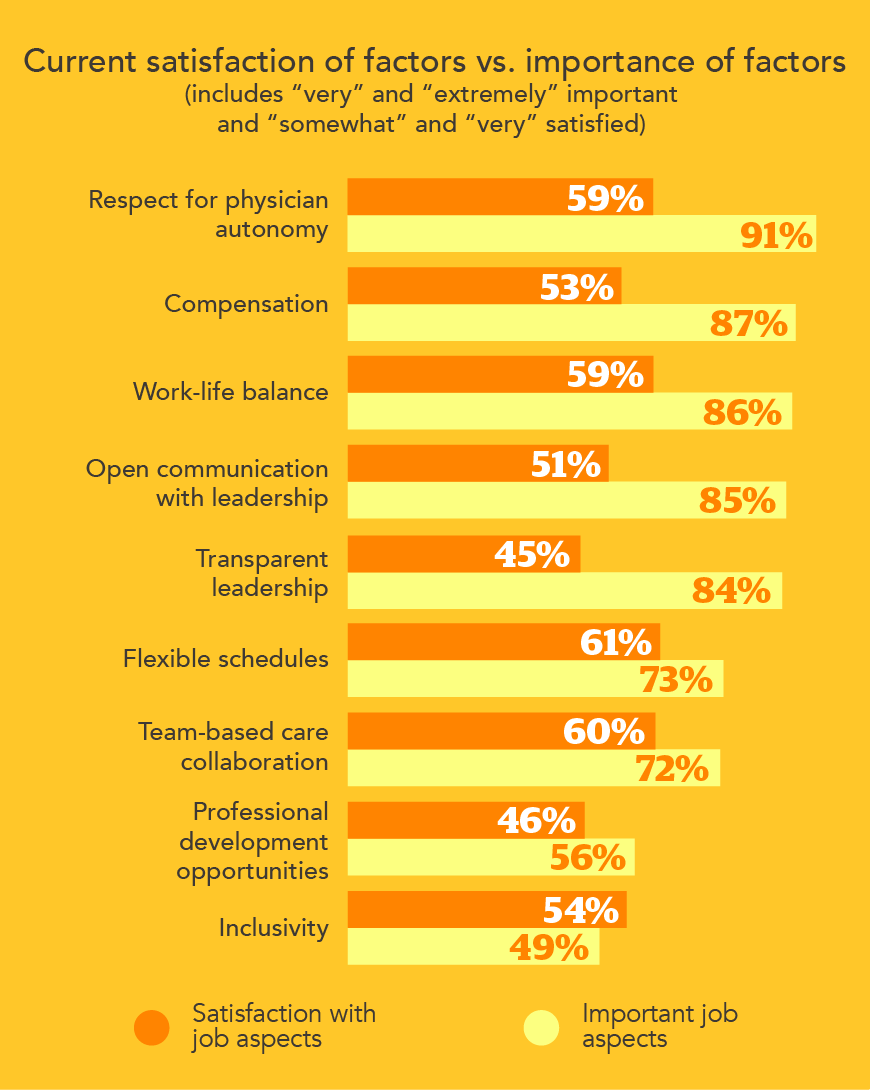
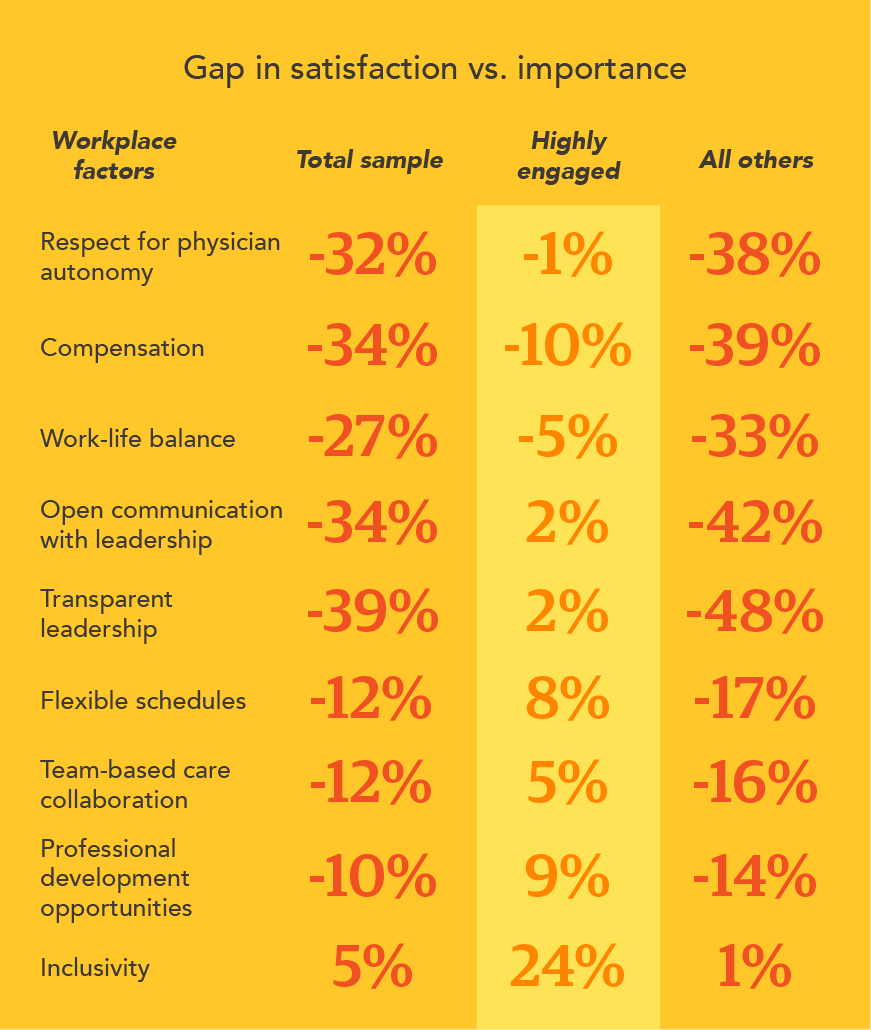
Highly engaged physicians were more likely to be satisfied across the board with the factors that are important to them, including leadership. While factors like compensation and physician autonomy rank highest in importance, they are often shaped by broader organizational and market forces. In contrast, transparent leadership and open communication—which also rank highly—are well within leadership’s control and present immediate opportunities to strengthen physician engagement.
Physician concerns about the economy and public health landscape
Some aspects of a job may be more influenced by outside pressures than within the control of healthcare leaders. Physicians identified concerns about public health (44%), funding cuts (35%), Medicare and Medicaid fee cuts (33%), and prescription drug costs (33%) as the top factors creating volatility in their workplaces.

Highly engaged physicians reported lower concern across a range of workplace challenges. Highly engaged physicians were less impacted by staffing, funding, and supply reductions—or they may feel more supported by leadership, making those challenges seem less acute.
The economy is another cause of worry and concern for physicians, with 45% saying they are very or extremely concerned. Additionally, 65% said they have grown more concerned over the past year.
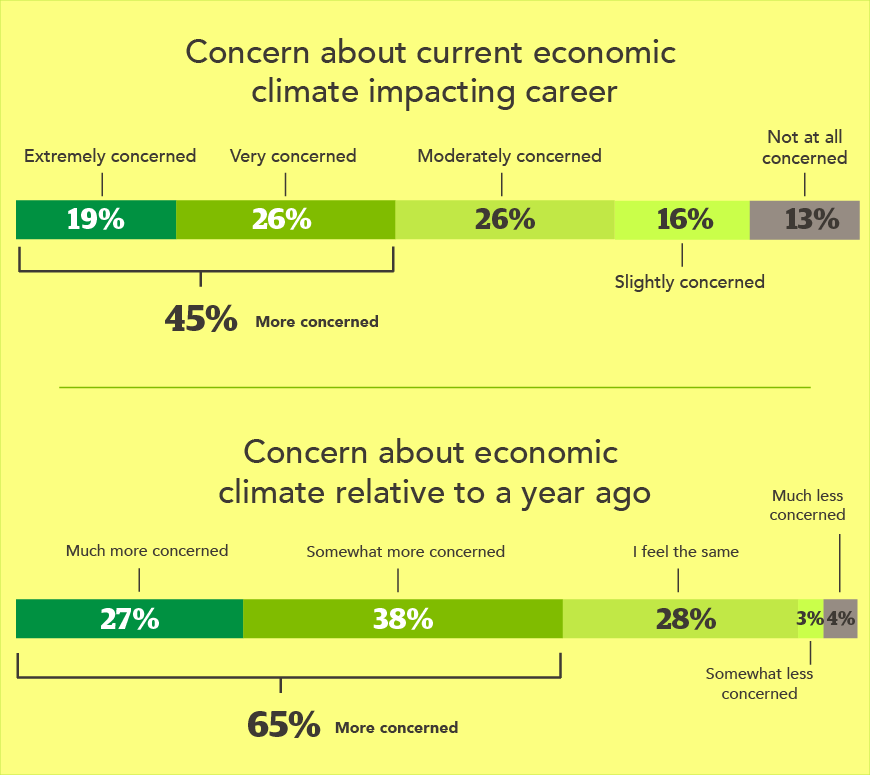
In response to these economic concerns, many physicians are looking for ways to improve their economic outlook or supplement their income. For example, 31% plan to explore additional work not related to medicine, while 30% plan to supplement their income by moonlighting. For physicians who currently work locum tenens, almost half intend to work more days.
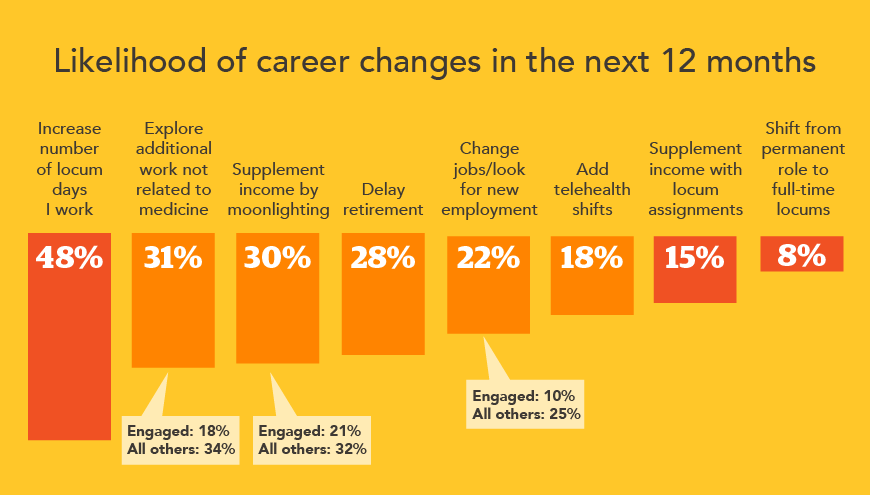
Of note, highly engaged physicians are much less likely to seek work outside of medicine, moonlight, or look for new employment. Only 10% of highly engaged physicians plan to change jobs, while 25% of all others plan to do so.
Top challenges in the healthcare workplace
The 2025 CHG Healthcare Physician Sentiment Survey explored workplace challenges using both quantitative questions to measure prevalence and qualitative questions to reveal deeper insights and nuance.
Quantitative: The challenges identified by physicians point to a significant burden from documentation and administrative tasks, as well as overall high workloads. Many noted challenges related to leadership not listening to physicians (34%) and a lack of transparency (27%). However, highly engaged physicians were significantly less likely to identify with these problems (8% and 4% respectively).

Qualitative: Respondents who had indicated that they were at least slightly likely to change jobs were given an opportunity to describe their workplace challenges in their own words. An analysis of these responses found that “workload and staffing” and “administration and bureaucracy” were the most prevalent themes in these open-ended comments.
“Non-physician administration is adversarial and dishonest with the physicians,” according to one respondent. Another describes the challenge as, “Administration not respecting what our department does and sets unrealistic goals and metrics.”
The significant gap between highly engaged and all other physicians in terms of feeling heard by leadership and perceived transparency in decision-making highlights the key role leadership plays in fostering satisfaction and engagement.
Physician perceptions of leadership
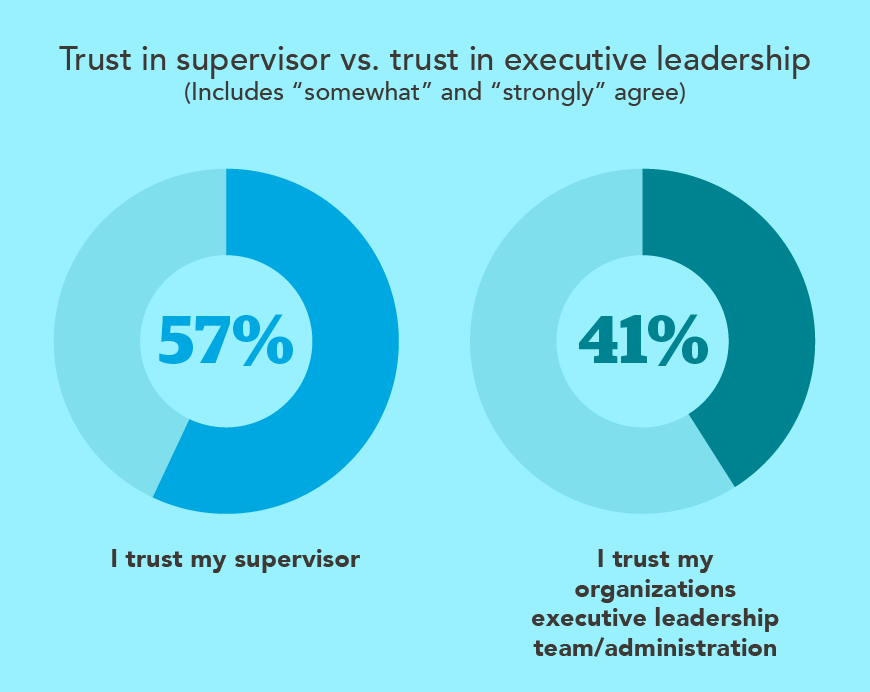
Physicians, regardless of engagement cohort, consistently report more favorable perceptions of their direct supervisors compared to executive leadership, highlighting the critical role of frontline leaders. Still, there is room for improvement in visibility, transparency, and connection throughout the organization. Two-thirds of physicians say their supervisors treat them with fairness and respect, while 57% say they trust their supervisor. In contrast, only two in five (41%) indicate they trust their organization’s executive leadership, feel aligned with leadership decisions, or believe their leadership communicates with transparency.

Opportunities for physician input in decision-making
Nearly three-quarters of physicians say they want to have input into decisions that affect their day-to-day work. But that desire is not being met—only 40% say executive leadership actively solicits physician input. That number is somewhat higher (48%) for supervisors. Even so, most physicians don’t believe their input is incorporated into leadership decision-making.

A stark difference emerges between highly engaged physicians and all others. A full 90% of highly engaged physicians report that their executive leadership actively seeks their input and, crucially, incorporates that feedback into their decisions.
However, this trust gap isn't inevitable; it's addressable. The higher trust ratings for direct supervisors demonstrate that physicians respond positively to accessible, visible leadership. Executive leaders face additional challenges in maintaining that visibility across larger organizations, but the principle remains: proximity, transparency, and demonstrated investment in physician perspectives build trust.
Feedback mechanisms
The survey results show a clear preference for regular, face-to-face meetings over more sporadic or formalized methods of providing input. Employee experience surveys are nearly as prevalent as face-to-face meetings, but physicians tend to dislike this feedback method. Creating more opportunities for personal, consistent feedback may lead to greater physician engagement.

The preference for face-to-face meetings over surveys reveals something important: physicians want dialogue, not just data collection. Surveys often feel transactional, whereas meetings tend to feel collaborative. This suggests that meaningful engagement isn't about having the perfect formal process—it's about creating regular, authentic opportunities for conversation where physicians feel heard and see their input shape outcomes.
Top physician priorities
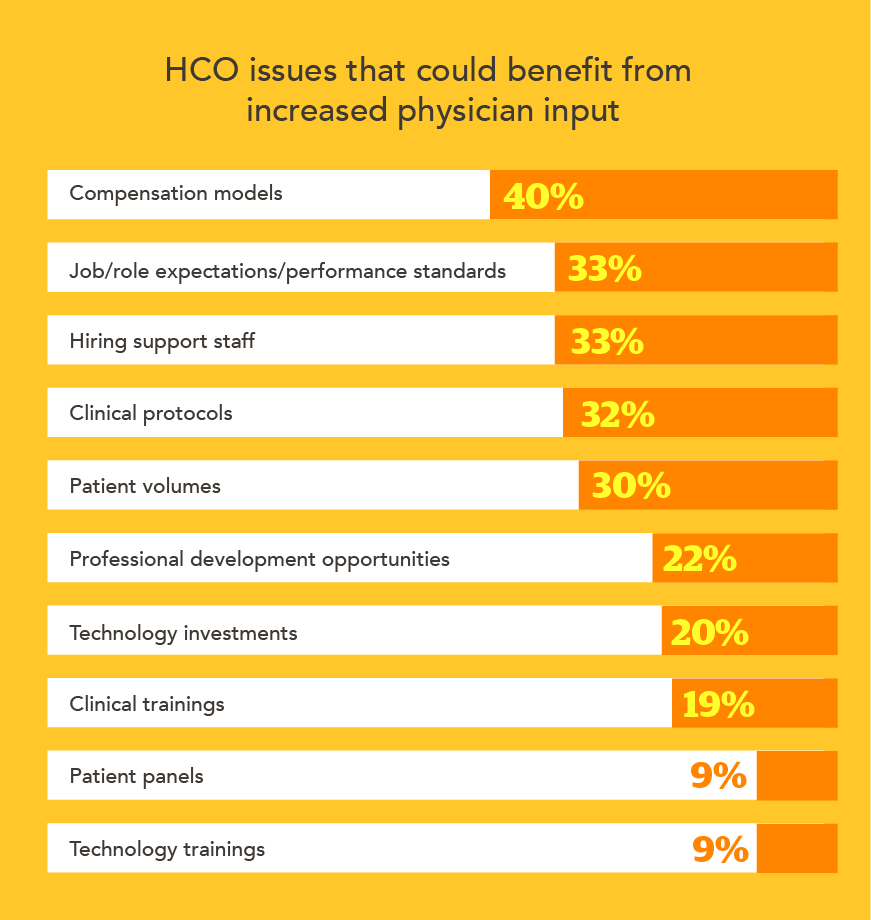
Physicians were asked to identify the issues that would most benefit from physician input, and their priorities show that physicians want a real voice in the decisions that impact their careers and their daily work. Notable priorities include compensation models and job/role expectations—areas that correlate to feelings of autonomy and professional satisfaction.
The demands of physician work in 2025
Physicians continue to work long hours, averaging 45 hours per week on scheduled shifts and an additional 15 hours on administrative tasks.
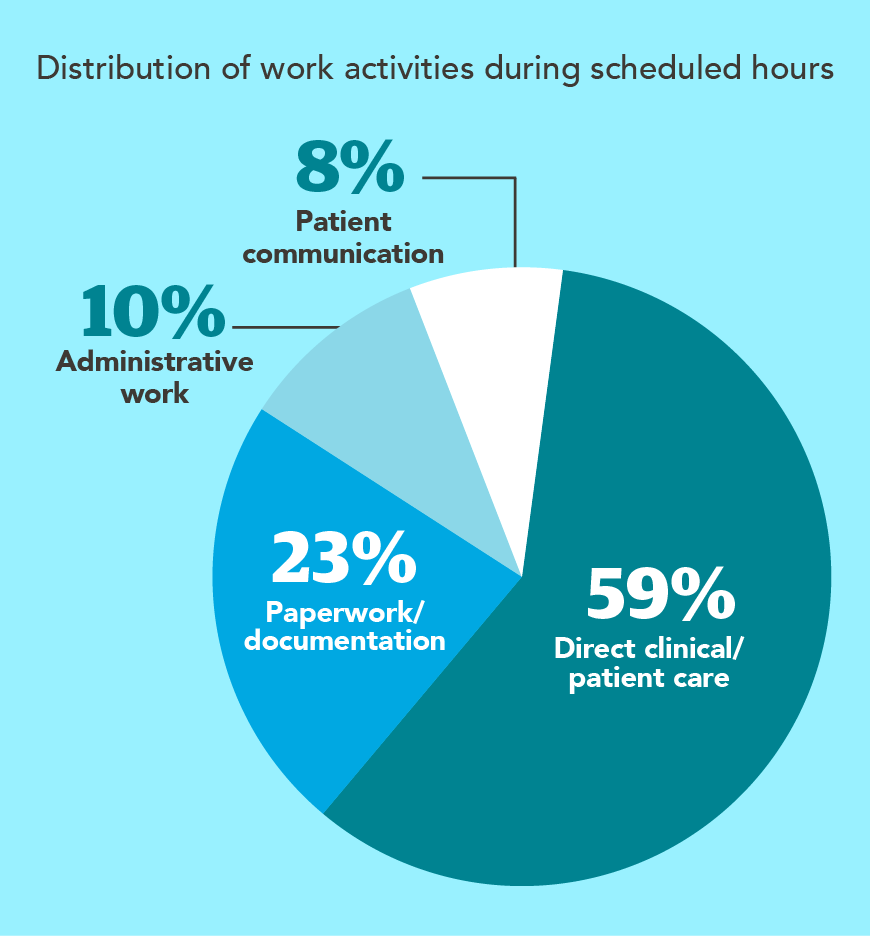
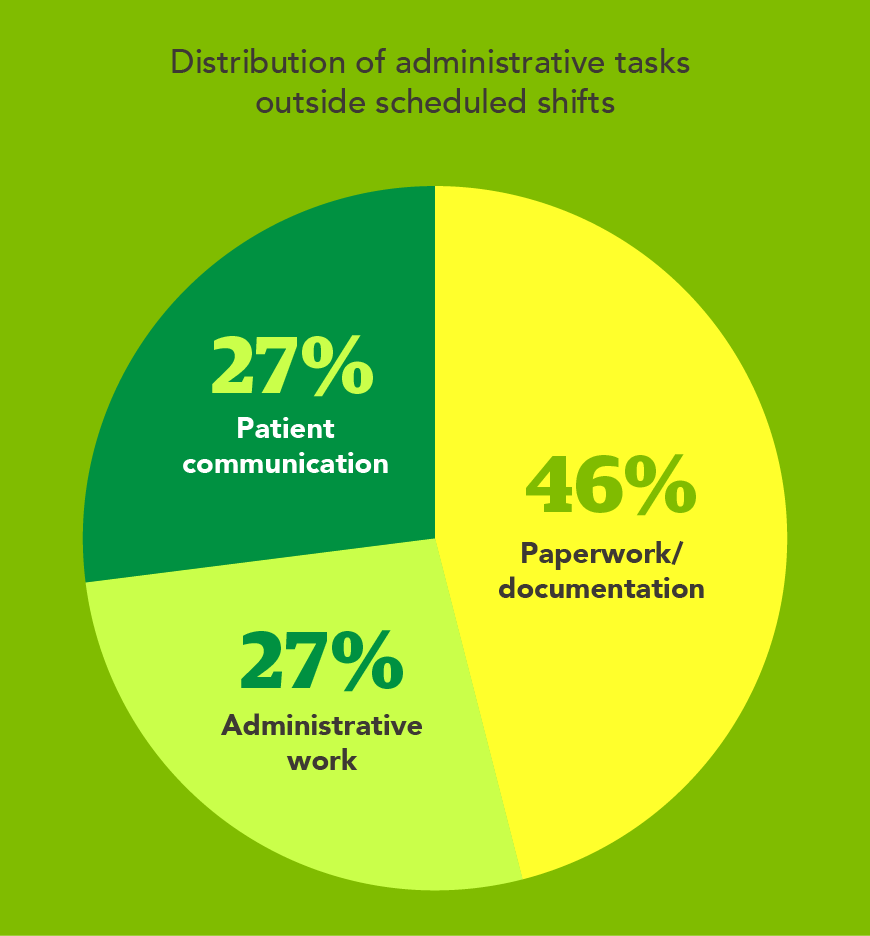
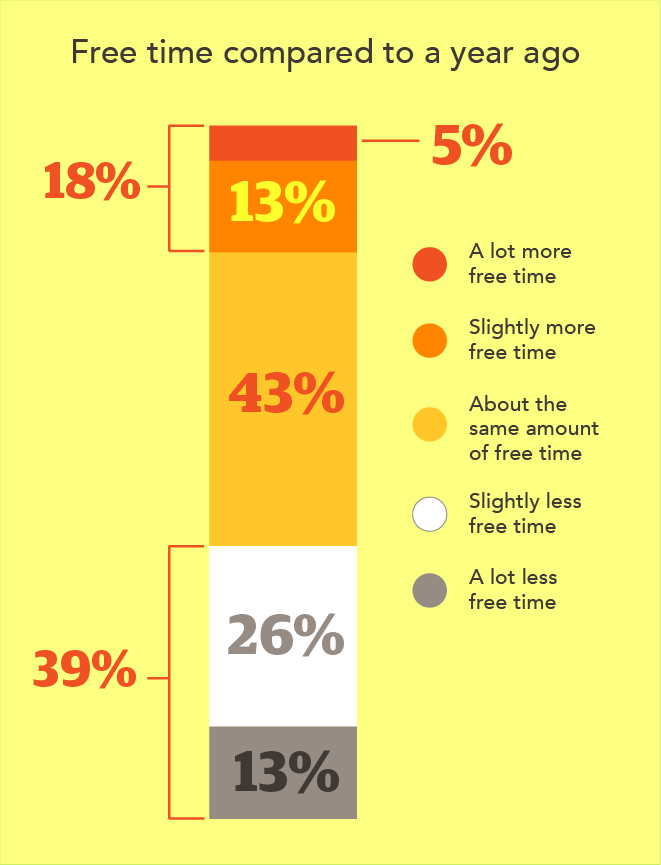
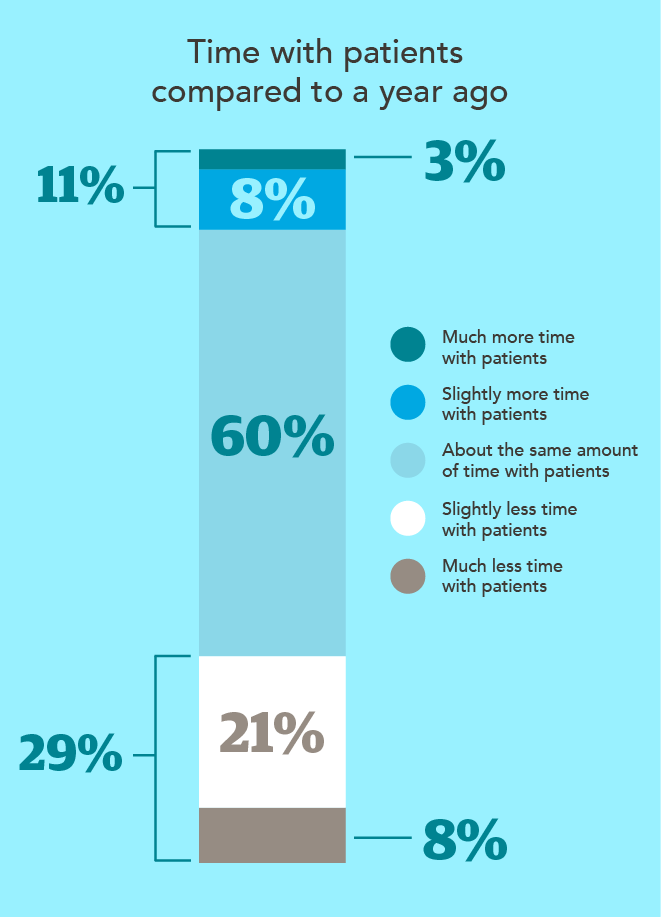
These tasks—charting, documentation, and patient follow-ups—are depleting both their personal time and time spent with patients. Nearly 40% say they have less free time than a year ago, and 28% say they spend less time with patients. These growing pressures are unsustainable and can lead to exhaustion and burnout.
Balancing priorities: Physicians and patients
Less than half of physicians (46%) believe that executive leaders implement policies with the best interests of patients in mind. Only a third (33%) believe that their leaders have physicians’ best interests in mind. Giving physicians input into the decision-making process and providing stronger communication and transparency around decisions can help build a culture where physicians feel supported and have a voice in decisions that impact patients. When physicians understand the 'why' behind leadership decisions—including the constraints leaders face—they're better equipped to align with organizational goals even when they might have chosen a different path themselves. This understanding builds trust and engagement without requiring perfect agreement on every decision.

AI and technology in healthcare
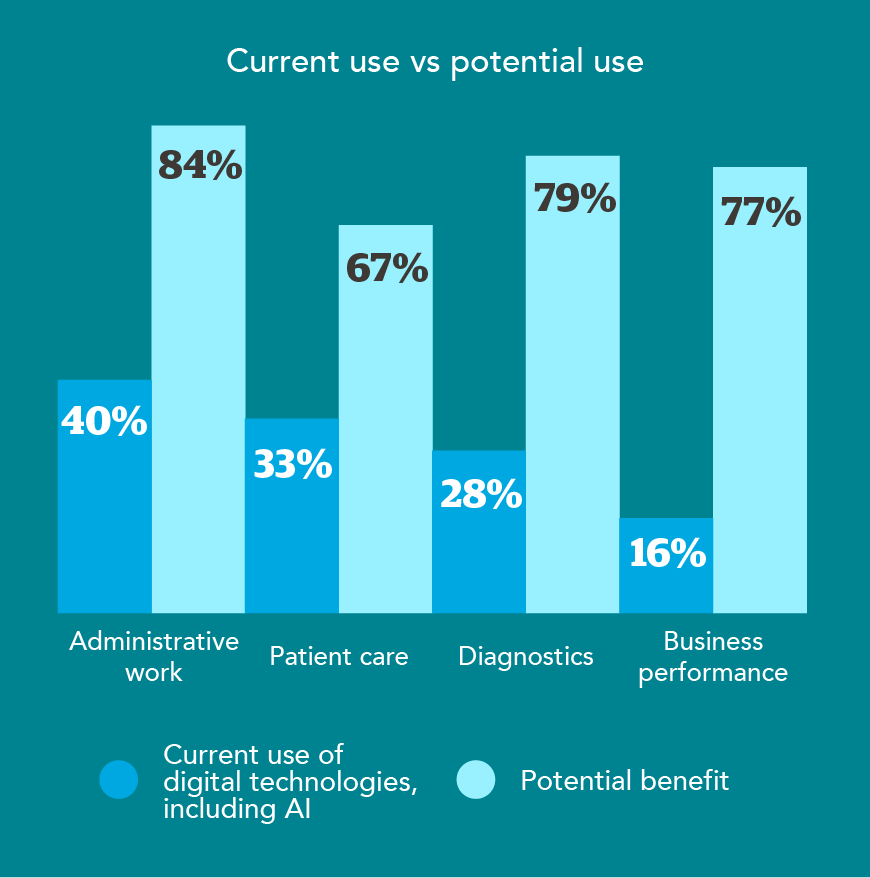
About 71% of physicians want to be involved in technology-related decisions. However, the vast majority feel excluded from these decisions, even though they see real potential for technology and artificial intelligence (AI) to help with administrative work, diagnostics, and business performance.
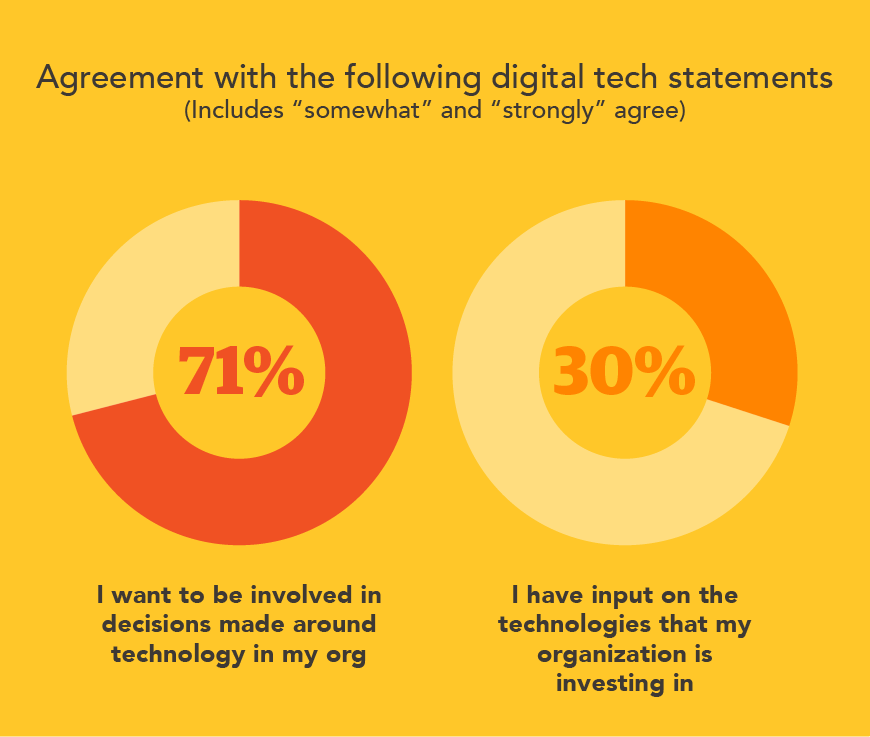
This disconnect—where physicians see AI's potential but feel excluded from decisions about its implementation—represents a missed opportunity. Including physicians in technology planning ensures solutions address actual pain points rather than creating new ones. More importantly, it demonstrates that leadership values physician expertise beyond the clinical domain, recognizing their practical insights about workflow, efficiency, and patient care delivery.
Reclaiming patient time in the Age of AI
With workloads and administrative burdens continuing to grow, physicians are placing hope in the potential of AI to alleviate some of the load. Roughly 70% say AI will improve their efficiency and productivity, while 57% believe it will have a positive impact on their workload.
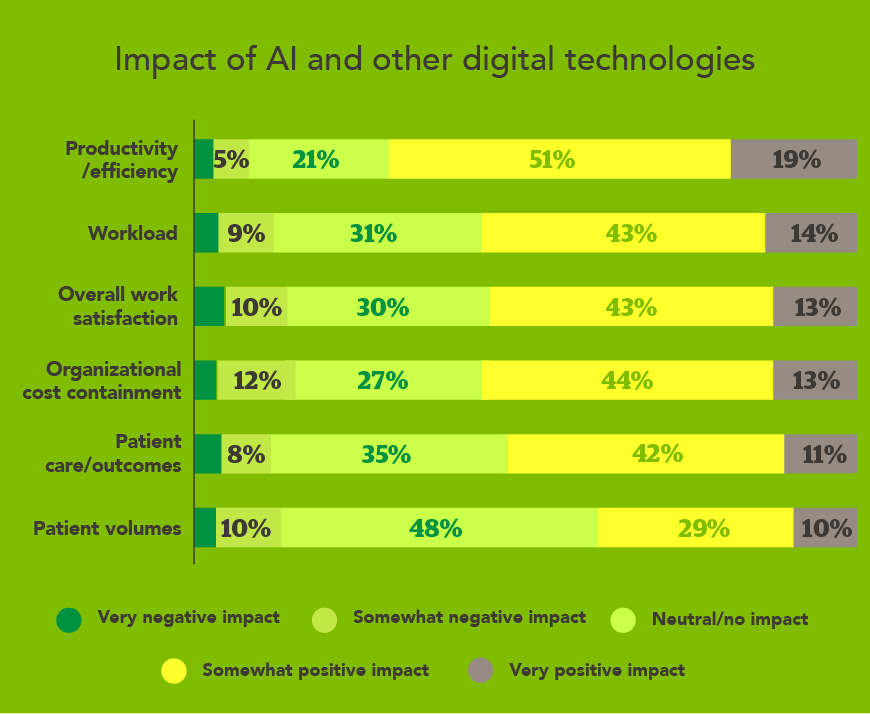
However, only 39% believe AI will have a positive impact on their patient volumes. Physicians are looking to AI to relieve their overwhelming administrative burden, not to increase their patient capacity. Similarly, only a minority of physicians agree that AI will help them spend more quality time with patients. Using efficiency gains to increase patient capacity—rather than reduce administrative burden—risks accelerating physician burnout and disengagement.

Closing the physician engagement gap: A roadmap for healthcare leadership
The findings from this survey reveal both a challenge and an opportunity for healthcare organizations. While 74% of physicians express satisfaction with their roles, only 18% are truly engaged—advocating for their organization, feeling connected to leadership, and planning to stay long-term. This gap represents significant organizational risk, but it also points to concrete, achievable solutions.
The role of leadership in physician engagement
The most striking finding in CHG’s research is the central role of leadership in driving physician engagement.
Highly engaged physicians differ from their peers in more than just their sentiments about compensation or workload—they have a different impression of their relationship with leadership.
- 90% report that executive leadership actively seeks and incorporates their input (compared to far lower rates among other physicians)
- They are 39 percentage points more likely to be satisfied with leadership transparency
- They are 34 points more likely to feel leadership communicates openly
- They are significantly less likely to cite leadership not listening (8% vs 34%) or lack of transparency (4% vs 27%) as challenges
This isn't about perfect working conditions or unlimited resources. Highly engaged physicians face the same market pressures, regulatory constraints, and economic uncertainties as their peers. The difference lies in their experience with leadership—factors that healthcare leaders can directly influence.
Actionable strategies: What healthcare leaders can do now
The disconnect between physicians and healthcare executives is real, but it’s a problem that can be solved. Data shows that many of the most impactful improvements don't require budget increases, policy overhauls, or organizational restructuring; they require intentional, consistent leadership practices.
1. Increase visibility and transparency in decision-making
Physicians trust their direct supervisors (66%) far more than executive leadership (41%), suggesting a gap in executive visibility. Only 40% feel executive leadership actively solicits their input, yet 74% want to provide it.
Implementation approach: Establish regular touchpoints between executive leadership and physicians—not just formal surveys, but face-to-face meetings, which physicians prefer.
2. Explain the "why" behind decisions
Physicians want to understand the business rationale for decisions that affect their work. This doesn't mean physicians must agree with every decision, but understanding the reasoning builds trust and alignment.
Implementation approach: When implementing changes, communicate not just what's changing, but why—including the constraints and trade-offs leadership is navigating.
3. Create meaningful opportunities for physician input
71% of physicians want involvement in technology decisions, yet most feel excluded. Top priorities for physician input include compensation models, job expectations, and technology implementation—all areas where the physician perspective adds strategic value.
Implementation approach: Identify two to three upcoming decisions where physician input could genuinely shape outcomes, and create structured ways to gather and incorporate that feedback.
4. Demonstrate that physician input matters
It's not enough to ask for input; physicians need to see it reflected in their decisions. When physician feedback can't be implemented, explaining why protects trust.
Implementation approach: Close the feedback loop by sharing how physician input influenced recent decisions or, when not possible, why certain constraints prevented implementation
5. Leverage AI and technology with physician partnership
Physicians see AI's potential to reduce administrative burden (70% expect improved efficiency), but worry gains will be used to increase patient volumes rather than reclaim their time. Including physicians in technology decisions ensures implementations address their actual needs.
Implementation approach: For AI and technology initiatives, engage physicians from the planning stage—not just implementation—to ensure solutions truly reduce burden rather than redistribute it
The business case for engagement
These leadership practices aren't just about physician satisfaction—they're about organizational performance. Highly engaged physicians are:
- More than twice as likely to stay (only 10% plan to change jobs vs 25% of others)
- Less likely to seek supplemental income outside their primary role
- More resilient to external pressures and workplace challenges
- Better advocates for their organization in recruitment and reputation
In a healthcare landscape facing economic uncertainty, workforce shortages, and mounting regulatory pressures, physician engagement isn't a nice-to-have—it's a competitive advantage.
Methodology
The 2025 CHG Healthcare Physician Sentiments Survey was conducted in May 2025 by Hanover Research for CHG Healthcare. The study was fielded in May of 2025 and captured responses from 920 physicians currently practicing medicine within the U.S. healthcare system.
Strengthen physician engagement at your organization
Connect with a CHG Healthcare physician workforce strategist to discuss how these findings apply to your specific situation and explore strategies tailored to your needs. Call 866.570.9920 or ecs.contact@chghealthcare.com to learn more.