
Physician turnover isn’t a new challenge, but for many healthcare organizations, it’s becoming more urgent, thanks to tight budgets, growing patient needs, and a shrinking workforce.
High turnover rates hurt healthcare organizations. Recruiting, onboarding, and training new physicians and advanced practice providers (APPs) is expensive, but the cost goes beyond the financial. Turnover also disrupts continuity of care, undermines morale, and can even lead to poorer patient outcomes.
For healthcare executives balancing tight budgets and rising patient demands, physician turnover can quickly erode both care quality and financial performance.
Meanwhile, demand continues to rise: The population is expanding, and patients are older and sicker. By 2036, the U.S. population of those 65 and older is projected to grow by 34.1%, with an increase of 54.7% in the 75 and older cohort.
And because physicians are not immune to aging, many are now approaching retirement. Demand is outpacing supply, and it’s only going to get worse. According to 2024 data from the Association of American Medical Colleges, the US could face a physician shortage of up to 86,000 physicians by 2036.
So, how can healthcare organizations keep talent and minimize attrition? Here are eight strategies to improve physician retention and reduce burnout.
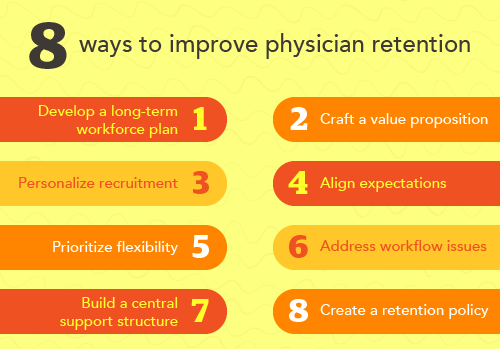
1. Develop a long-term physician workforce plan
Do you know what your physician workforce needs will be in the next five years? Start by building a three-to-five-year roadmap using such data as population trends, zip codes, patient demographics, and current provider capacity.
Planning ahead helps align physician supply with projected care needs. It also reduces the risk of last-minute, possibly ill-advised, hiring decisions.
“You’d be surprised how many organizations don’t have a plan like that,” says Scott Polenz, principal consultant of CHG Healthcare’s Advisory Services. Without one, they could face unnecessary shortages and avoidable stress on clinical teams, which can hurt retention.
Hire smarter: Strategic recruitment of physicians in an increasingly competitive market
2. Craft a compelling value proposition
Why should a physician choose your organization? Why should they stay?
Develop a strong value statement that clearly communicates your mission, culture, and support systems—not just your compensation package. This message should be consistent across your recruiting, onboarding, and day-to-day operations. A compelling value proposition attracts top talent who share your mission and vision and helps them feel connected long after the contract is signed.
3. Personalize physician recruitment and onboarding
Make recruitment personal, not transactional. Treat physicians and their families as individual people, not merely potential hires.
Polenz shares a story about recruiting a physician to a rural facility—often a tough sell. Over dinner, he noticed the physician and his wife each added four creamers to their coffee. “That night I asked my assistant to go find the biggest box of creamers that you could find, and we hand-delivered it the next day with a note saying, ‘We’ll make sure you have all the creamers you’ll ever want.’”
It worked; the doctor signed.
“You have to personalize it,” he says. “Make it unique. They need to feel like, ‘If I come work for this organization, they’re going to treat me like family.’”

Too often, he adds, healthcare organizations treat physicians like commodities. “They're not commodities—they're brilliant human beings. They're not widgets.” Personalized onboarding is among the top physician recruitment best practices and a smart retention tool as well.
Create a stronger team: How to address staffing challenges by creating a flexible physician workforce
4. Align expectations internally
Before launching a search, the entire clinical team—physicians, administrators, and support staff—should be aligned on key expectations such as call schedules, RVU targets, partnership timelines, workload distribution, and organizational culture.
Put these expectations in writing and ensure everyone involved in the interview process shares a consistent message. Polenz offers some suggestions: “Call is one in four. RVU expectations are X. Here’s how the partnership works.”
This kind of cohesion builds trust with candidates. If even one physician expresses doubt—or seems resistant to a new hire—it can send mixed signals and derail the process. “If your team isn’t aligned,” Polenz says, “you probably shouldn’t be recruiting yet.”
It’s a reminder that physician recruitment best practices are also physician retention best practices, too.
Align to engage: The secrets to long-term physician retention
5. Prioritize flexibility and autonomy
Physicians want control over how they work, when they work, and how they care for patients. Giving them flexibility and autonomy can significantly reduce burnout and boost retention. They also demonstrate that your organization trusts its physicians.
Flexibility may mean different things to different people, but here are a few options:
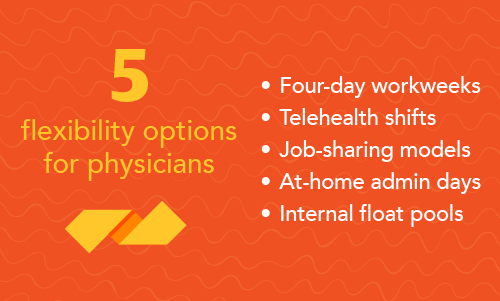
- Four-day workweeks
- Telehealth opportunities
- Job-sharing models
- At-home administrative days
- Internal float pools that allow physicians to take on extra shifts internally rather than look for outside work
Many healthcare organizations are successfully implementing flexible work schedules. It largely comes down to trust, Polenz says. For example, if a physician has a 0.2 administrative role, why not let them work from home one day a week? That kind of trust signals respect and strengthens engagement.
Polenz adds that all this advice about flexibility, trust, and autonomy applies to advanced practice providers as well.
Try something new: Adapting compensation to support flexibility and improve retention
6. Address workflow headaches
Physicians are often overwhelmed by administrative burdens, which are made worse by rigid scheduling and staffing gaps.
A report published in the Journal of the American Board of Family Medicine supports Polenz’s observations and recommends the following approaches to help retain physicians:
- Distribute documentation and workload more evenly across care teams.
- Ensure adequate staffing across all clinical and support roles.
- Provide better training and support for EHRs.
- Assign administrative tasks, such as inbox management and documentation, to other team members.
Physicians shouldn’t spend their time doing work that others on the team could handle more efficiently. Delegating these tasks frees up time for patient care, reduces stress, and improves job satisfaction.
7. Build a centralized physician support infrastructure
Create a unified hub—an office of physician and APP relations— that combines onboarding, HR, credentialing, well-being, mentorship, and recognition under one umbrella.
Too often, physicians are forced to chase down answers across multiple departments. While HR may be able to provide compensation details or evaluation timelines, physicians frequently need to navigate different teams for credentialing, burnout support, or administrative help.
Creating a “one-stop shop” makes life easier for physicians and APPs, Polenz says. It improves retention, builds trust and ensures better alignment across the organization.
He points to another benefit: Physicians also want to grow in their careers—not just clinically, but as leaders. A centralized support structure can point them toward professional development opportunities and structured mentorship.
Use new tools: A guide to using AI to enhance the physician recruiting process
8. Create a formal physician retention policy
Despite the high cost of turnover, only 23% of healthcare organizations surveyed had a formal retention policy, according to an Association for Advancing Physician and Provider Recruitment report.
“We do a really good job in healthcare of bringing them on,” Polenz says. But without follow-up and a focus on retention, the doctor who was so heavily recruited ends up feeling forgotten.
A formal retention strategy should include measurable efforts across several key areas:
- Culture and leadership communication
- Practice efficiency and workflow
- Collegiality and social connection
- Professional growth, recognition, and well-being
Polenz emphasizes that these efforts aren’t merely feel-good initiatives; they have a tangible financial return. Fully engaged physicians are 26% more productive, generating nearly $500,000 more in annual revenue, he says.
What physicians say: 2025 Physician Sentiment Survey
It’s never one thing: It’s everything
When physicians decide to leave, it’s rarely because of a single issue. As researchers write in the Journal of the American Board of Family Medicine, these decisions are shaped by "multiple interdependent factors," including better compensation. But for many of those surveyed, higher compensation alone wouldn’t have convinced them to stay.
You won’t be able to tweak a few numbers and improve retention. Retention should be top of mind during recruitment and starts in earnest with onboarding.
Polenz warns that some CFOs may dismiss retention and engagement efforts as “touchy-feely” or nonessential. But he says the numbers tell a different story: Engaged physicians are more productive, and replacing just one physician can cost an organization as much as $1.2 million.
“Nobody walks into a hospital or clinic to see an administrator,” Polenz says. “They walk in to see their doctor and their care team.”
Physicians are not commodities—they are the core of patient care. Investing in their trust, autonomy, and sense of purpose pays off in outcomes, stability, and loyalty. They’re not just your workforce, they’re the heart of your organization.
Download a one-page summary of this article by clicking the image below:

CHG can provide your healthcare facility with the doctors, advanced practice, and allied professionals you need to provide the best care for your community. Contact us at 866.570.9920 or email ecs.contact@chghealthcare.com.