
When patients feel confident that they’re getting the best care at a healthcare facility, they are likely to return again and again, and a positive relationship can make the difference between a one-time visit and a decades-long connection. Calculating the lifetime value of your patients allows you to quantify how positive patient experiences impact the bottom line, which can help you build the business case for initiatives to improve the patient experience.
How to calculate patient lifetime value
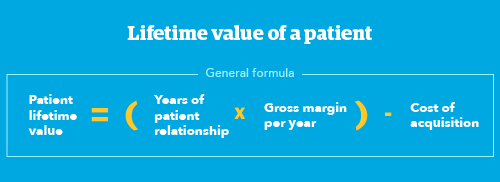
You can put an actual number on the lifetime value of your patients. While the total for one year may not look very impressive, when you project five, ten, or 25 years into the future, you begin to see each patient's true lifetime value. Here’s the formula in the simplest terms:
Patient lifetime value = (Years of patient relationship x Gross margin per year) - Cost of acquisition
However, there are a lot of factors that go into calculating the true patient lifetime value. Here’s how to calculate it.
1. Gather patient revenue and cost numbers
Before starting your patient lifetime value calculation, you’ll need the following:
Average revenue per patient per year: This amount should consider both reimbursements and utilization (which is affected by factors such as population size, system growth, and patient loyalty).
Operating costs per patient per year: This includes care delivery costs and non-care delivery costs, like a contact center. To reduce these costs, reduce redundancies and service bottlenecks for more efficiency.
Average operating margin rate: This rate is determined by dividing the difference between net patient revenue and total operating costs by the net patient revenue.
(Net Patient Revenue – Total Operating Costs) / Net Patient Revenue = Average Operating Margin Rate
2. Calculate gross margin per patient
Next, determine the gross annual profit margin of an average patient by multiplying the average revenue per patient by the average operating margin rate. Here’s the equation:
Average Revenue Per Patient ($) x Average Operating Margin Rate (%) = Gross Margin per Patient
So, if your average revenue per patient is $20,000 per year and your average operating margin rate is 2.92%, your gross margin per patient would be $584.
$20,000 x .0292 = $584
3. Calculate net revenue per patient
Next, subtract the patient acquisition cost per patient to get your net revenue per patient. Patient acquisition costs include marketing campaigns and community outreach. Higher patient satisfaction and retention rates can lower these costs. So, if your acquisition cost is $400 per patient, the calculation would look like this:
$584 - $400 = $184
However, the net revenue per patient above is only for one year. So, the patient lifetime value equation is actually this:
(Years of Patient Relationship x Gross Margin per Year) - Cost of Acquisition = Patient Lifetime Value
Or using our example numbers above:
(1 x $584) - $400 = $184
4. Calculate the patient lifetime value
However, calculating actual lifetime value is complicated because the dollar value increases over time to account for inflation and other future financial benefits. As a result, you need to calculate the present value of the patient over time. So, the formula becomes:
Present Value of the Patient Over Time - Cost of Acquisition = Patient Lifetime Value
Use the following Excel formula to find the present value over time:
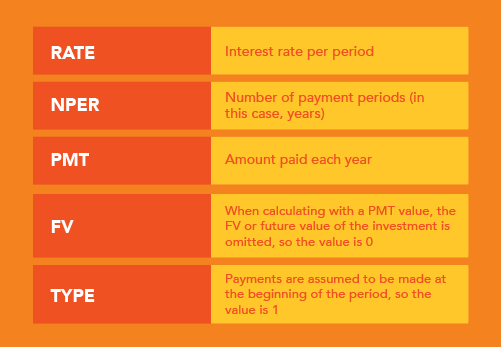
= -1*PV(RATE, NPER, PMT, FV, TYPE)
Here’s an explanation of the values you would need to identify for each field:
When calculating patient lifetime value, it might look like this:
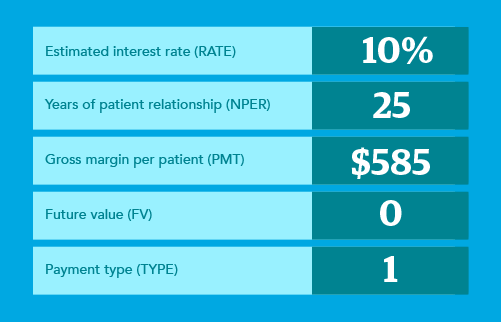
Using this formula, the lifetime value for one patient over 25 years would be:
-1*PV(.10, 25, 584, 0, 1) - 400 = $5,431.09
When you multiply by the number of patients, the value is even more impressive!
Patient Lifetime Value Over Time x # of Patients = Total Value
So, if you have 10,000 patients, the total value in our example would be:
- 1 year = $1.84 million
- 10 years = $35.5 million
- 25 years = $54.3 million

Understanding the factors behind patient lifetime value
Years of patient relationship
Naturally, the longer a patient has a relationship with your institution, the more value they bring.
Positive experience: Creating a positive experience for patients builds loyalty, which leads to increased utilization and word-of-mouth advertising.
Patient retention rate: The higher that retention rate, the bigger the impact on your patient’s lifetime value. Measuring the patient retention rate is key because knowing that rate will help you understand how much effort you’ll need to put into improving the patient experience.
Gross margin per year
Gross margin looks at both how much revenue is generated from repeat or continuous utilization over time and identification areas where there could be cost savings.
Revenue: This money comes from increased utilization — which can come from population or system growth as well as patient loyalty — and reimbursements. Notably, patient satisfaction scores, such as from the HCAHPS survey, can affect reimbursement rates. So, the patience experience piece on the revenue front is critical.
Service costs: Learning about your patients’ experience can help reduce service costs. It can uncover redundancies and bureaucratic barriers that frustrate patients, uncovering bottlenecks and increasing efficiency.
Increase your reimbursement revenue: 7 ways to improve your locums payor enrollment process
Cost of acquisition
The final piece of the equation is factoring in costs related to patient acquisition, such as marketing campaigns or community outreach. Again, patient experience impacts this number as well. A patient tends to tell people if they’ve had a negative experience. They’ll tell many people about a positive experience, but they tell even more people about a negative one.
How patient experience impacts the bottom line
It’s a simple connection: Positive patient experience leads to longer patient relationships. Additionally, happy patients will spread the word to their family and friends.
“When you look at the lifetime value of a patient, experience makes all the difference in the world,” says Kristin Baird, president and CEO of The Baird Group, a consulting company that helps make healthcare better for both patients and the people who serve them. “Experience is a retention strategy. When the experience is good, they’re not only going to return, but they’re also going to talk very positively about it. So, you want to make sure that you’re creating an experience that will not just fail to offend people but really wows them into saying, ‘I trust them. I wouldn’t go anywhere else.’”

Maximize patient lifetime value by maximizing patient experience
Patient experience feedback can enable you to make changes in the moment, so the next patient has a better experience. It’s important to create a mechanism that empowers continuous improvement and continuous change. For healthcare leaders seeking to strengthen their organizations, it’s critical to double down on measuring and improving patient experience to build long-lasting patient relationships. Customer experience companies like Qualtrics can help you develop programs to continuously measure and improve the patient experience.
This article first appeared on WeatherbyHealthcare.com. Weatherby Healthcare is a division of CHG Healthcare. Let us know how we can support your facility’s staffing needs. Give us a call at 866.851.9214 or email ecs.contact@chghealthcare.com.