Executive summary
CHG Healthcare surveyed more than 1,200 physicians, nurse practitioners, physician assistants, and registered nurses to find out how COVID-19 has affected providers' career planning, satisfaction, and burnout, and asked about healthcare organizations' responses to the pandemic.
Career satisfaction is down
COVID-19 has greatly impacted the world, creating a healthcare crisis unlike anything seen in modern times. Healthcare workers have responded positively — often putting their own welfare aside to help others. While they have been giving everything to fight the pandemic, it is not surprising that 43% reported the pandemic as having a negative impact on their career satisfaction.
Burnout is getting worse
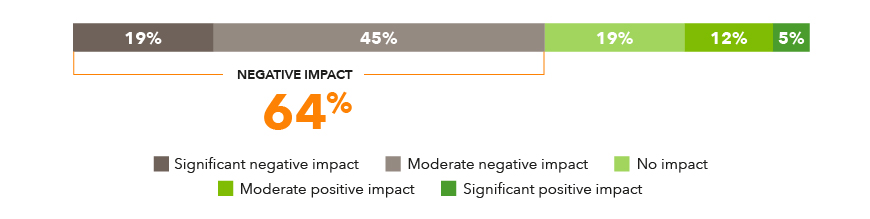
In addition to impacting career satisfaction, the pandemic has also impacted the amount of burnout providers are feeling. Before the pandemic, 80% of providers were suffering from some degree of burnout. Of those, 64% reported that the pandemic has made their burnout worse.
Employer response to COVID-19 is good
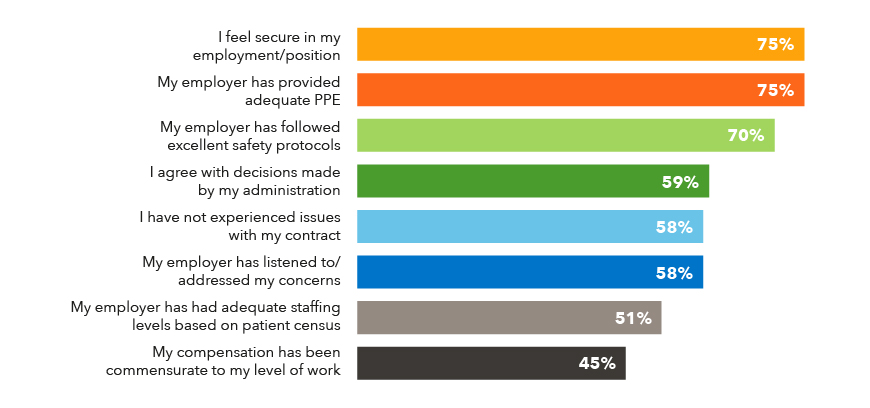
While career satisfaction and burnout were negatively impacted, most providers (69%) felt their employers did a good job responding to the pandemic. Most also felt that their jobs were secure (75%), they had sufficient PPE (75%) and that safety protocols were being followed (70%).
Staffing levels and compensation are too low
While the general response to the pandemic was positive, many providers felt there were areas where their organizations were lacking. When asked their top three concerns about their employers’ response to the pandemic, the leading issue was insufficient staffing levels, followed by dissatisfaction with compensation and inefficient work processes. Additionally, 22% reported that their employers did not listen to them and 26% indicated they did not agree with the decisions they were making.
Influences to career plans impacted by COVID-19
There are a wide variety of factors that impact how healthcare providers make career decisions. The most important things providers were looking for in their careers were work/life balance (83%), job stability (78%), and workplace culture (76%).
When asked which aspects of their career planning were most impacted by COVID-19, it is not surprising that workplace safety saw the most impact (75%). Job stability and work/life balance (both 65%) were the other top factors impacted by COVID-19.
Satisfaction with employer remains high but some are looking for new opportunities
Even with the drop in career satisfaction and increased burnout caused by COVID-19, the survey found most providers are planning to continue working in healthcare, with only 5% indicating it is unlikely they would continue in the field.
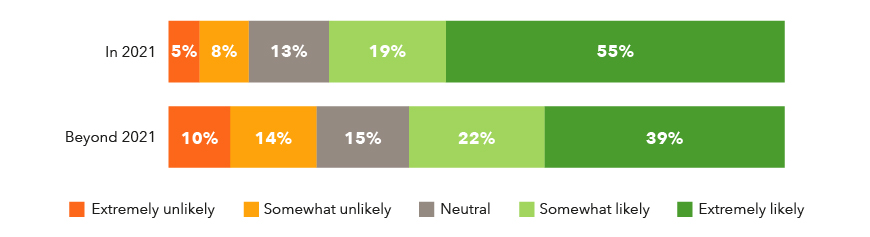
Additionally, the survey found most providers are planning to continue working in their current roles. However, the survey revealed that for some, that only held true for this year. Those who indicated they were unlikely to stay in their current roles jumped from 13% to 24% when asked if they would continue in their current role beyond 2021.
Survey report
Career satisfaction
When it comes to overall career satisfaction, 43% of all providers reported that COVID-19 has had a negative impact on their job.
COVID-19’s impact on career satisfaction
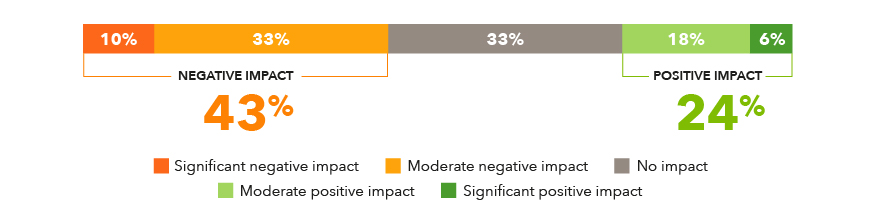
However, some specialties felt even more impact. 57% of physicians and nurses working in emergency medicine reported a negative impact and 67% of NP/PAs working in frontline roles (for this survey frontline roles include critical care, internal medicine, pulmonology, hospitalists, and infectious disease physicians). ICU and PICU nurses also reported negative impacts.
COVID-19 and Burnout
Along with career satisfaction, COVID-19 has also impacted the amount of burnout providers are feeling. Before the pandemic, about two-thirds of providers (63%) experienced slight to moderate burnout, and 18% were very or extremely burned out. Just 20% experienced no burnout at all.
Burnout levels - Pre-COVID-19
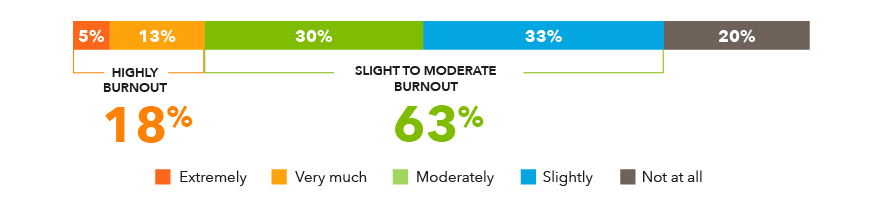
Unfortunately, 64% report that COVID-19 has negatively impacted their experience of burnout. And while 64% of all providers reported impacts to burnout, it was even higher for physicians working in frontline roles (75%) and emergency medicine (72%). It was also higher for NP/PAs working in OB/GYN (75%) and nurses working in frontline roles (77%) and emergency medicine (83%).
Impact of COVID-19 on burnout
Telemedicine and COVID-19
The telemedicine questions were only asked to physicians, PAs and NPs.
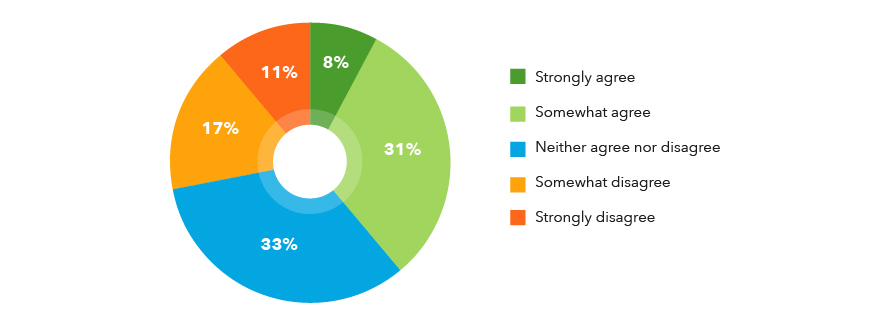
Working in telemedicine is one way some providers have found to reduce their burnout. There is a roughly equal split between providers who believe that telemedicine is an effective solution for reducing burnout (39%) and those who don’t (28%). Also, those who currently practice at least some telemedicine are more likely to agree that it is effective for reducing burnout.
Telemedicine’s effect on reducing provider burnout
Telemedicine has seen tremendous growth during the pandemic. Many organizations found themselves suddenly needing to use technology in order to keep seeing patients while maintaining proper safety protocols.
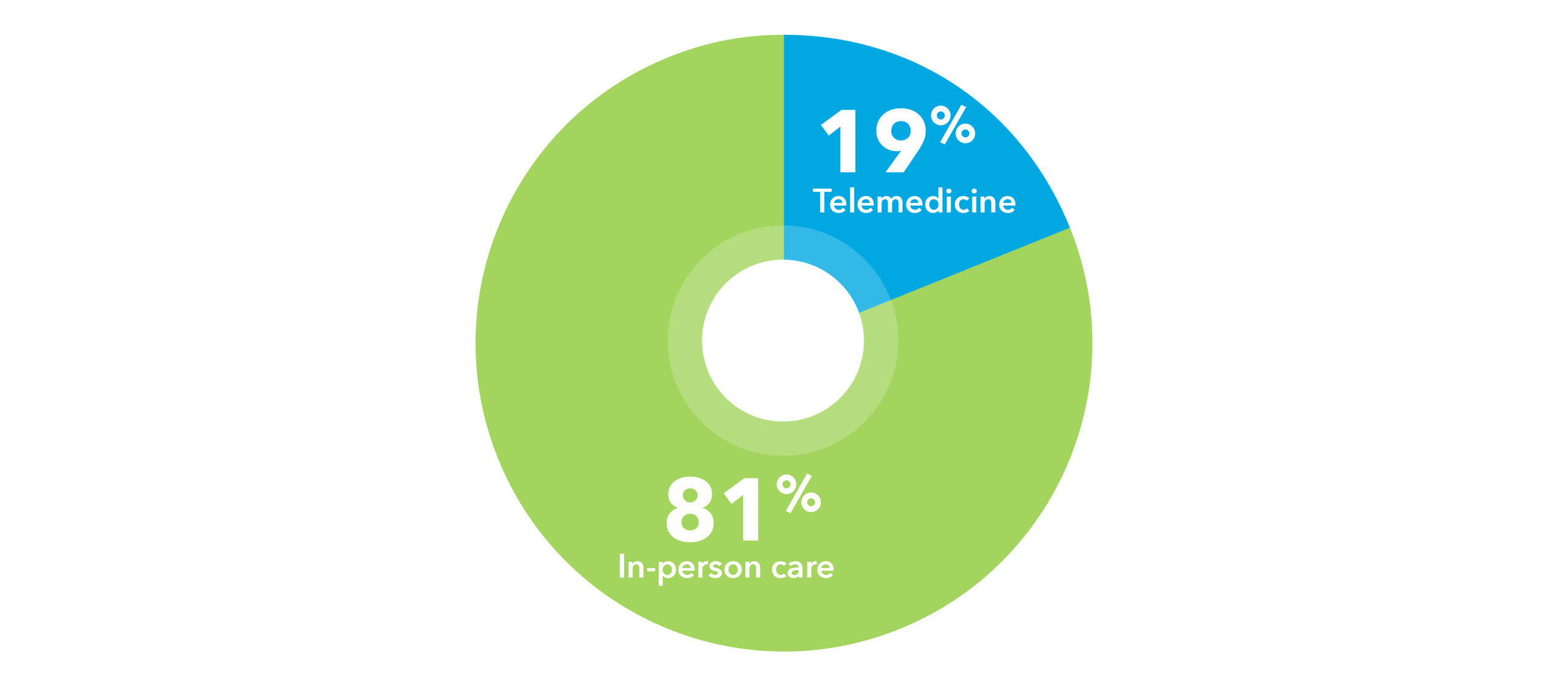
However, telemedicine still accounts for less than a quarter of a providers’ patient care even during the pandemic. The increase in telemedicine use has been primarily driven by providers who work in outpatient care settings, as those who work outpatient exclusively (27%) or jointly (16%) provide more telemedicine than those who exclusively work in inpatient settings (4%).
Recent in-person care versus telemedicine
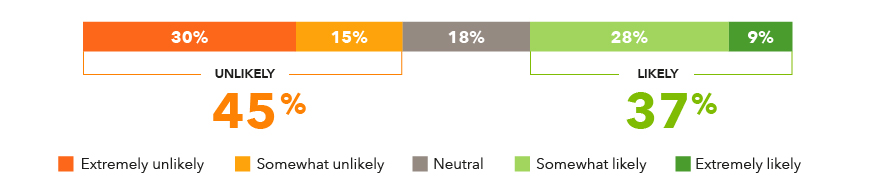
Of those who do not currently provide any patient care via telemedicine, about a third (37%) say they are likely to do so in the future, though the rest are either unlikely (45%) or neutral (18%).
Likelihood to provide telemedicine in the future
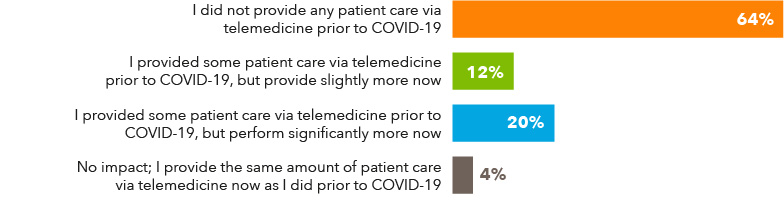
Of providers who practice at least some telemedicine, two-thirds (64%) did not have any experience before the pandemic, while a third (32%) had some previous experience but have reported an increase during COVID-19.
Impact of COVID-19 on telemedicine practices
Most providers (80%) who currently do at least some telemedicine expect to practice either the same amount or more in 2021 compared to 2020.
Future expectations
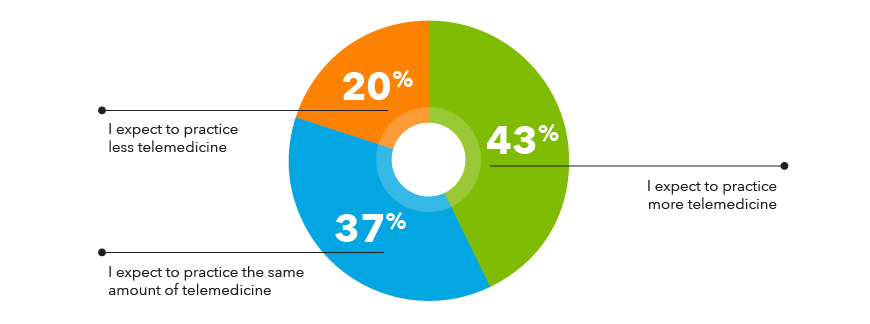
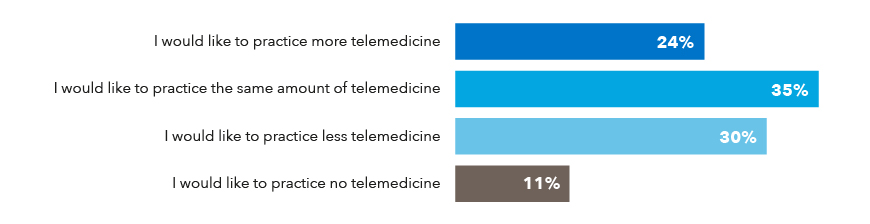
Interestingly, slightly over half of providers (59%) would like to practice the same amount or more telemedicine once COVID-19 is no longer a concern and the rest would prefer to practice less or no telemedicine (41%).
Ideal amount of telemedicine work post pandemic
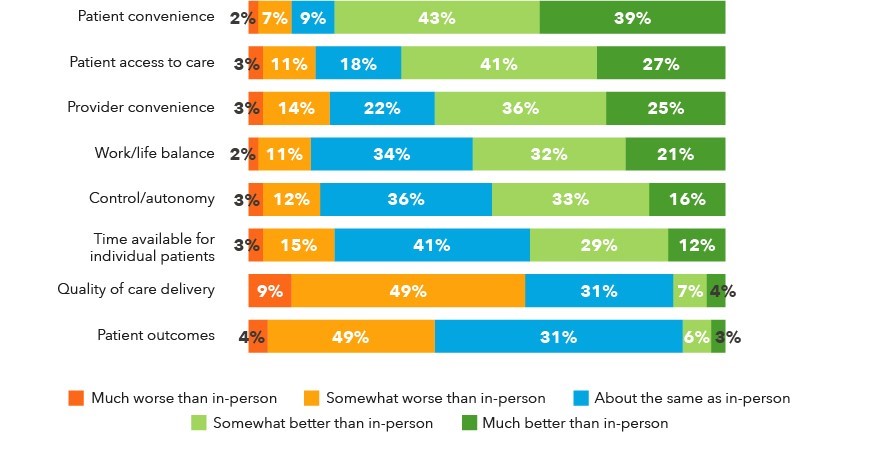
Telemedicine outperforms in-person care on patient convenience and access to care but underperforms on quality of care delivery and patient outcomes. Many also believe telemedicine is more convenient for providers (60%), allows for a better work-life balance (53%), and provides more control/autonomy (49%) compared to in-person care.
Evaluation of telemedicine based on key factors
Locum tenens and travel nursing impacts due to COVID-19
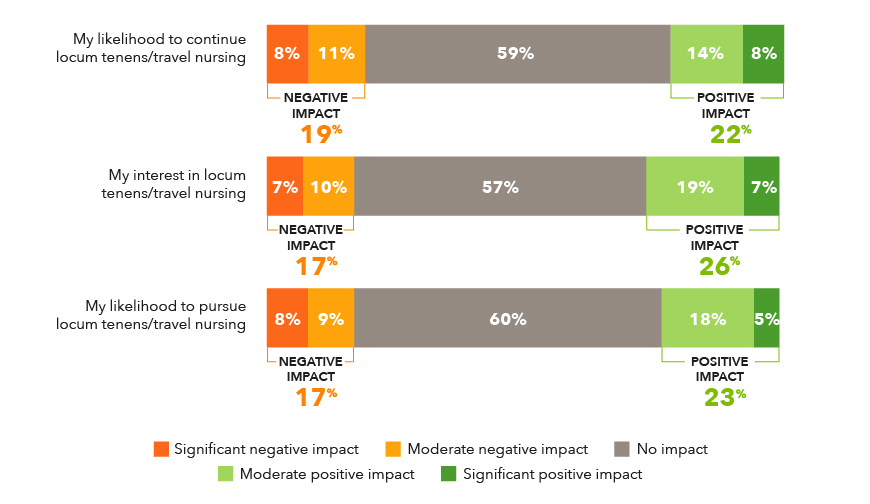
Telemedicine has proven to work for some providers. Locum tenens and travel work is another way some providers have found to make their career work for them. While the pandemic has impacted travel work, the negative impacts are less than the positive impacts, showing more providers are willing to look at this type of work.
Impact of COVID-19 on desire to continue or start locum tenens/travel nursing
Employer response to COVID-19
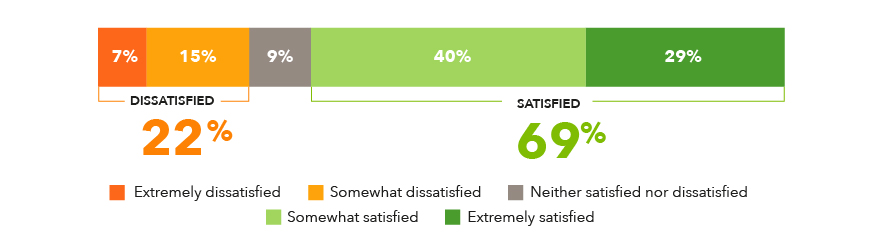
COVID-19 hasn’t just impacted individual providers and the way medicine is practiced. It has had huge impacts on healthcare systems and facilities around the country. The survey looked at how providers felt their organizations responded to the pandemic. Overall, most providers (69%) are satisfied with their employers’ response to COVID-19.
Satisfaction with employer’s COVID-19 response
Some job types and specialty groups, however, had stronger feelings of either satisfaction or dissatisfaction with fewer falling in-between. For example, 59% of physicians working in frontline specialties were satisfied while 31% were dissatisfied. Amongst NPs/PAs, of those in frontline specialties, 61% were satisfied and 35% were dissatisfied; in emergency medicine, 63% were satisfied and 38% were dissatisfied. Nurses in emergency medicine were equally split with 50% satisfied and 50% not.
The biggest negative reactions about employers’ responses to the pandemic were compensation and staffing levels. Overall, only 51% felt their employer had adequate staffing levels, and for nurses working in emergency medicine, the number dropped to just 17% with 78% feeling staffing levels were not adequate.
Also, only 45% of providers felt their compensation was commensurate to the level of their work. And while 58% felt their employers addressed their concerns, nearly a quarter felt they did not address their concerns. For physicians working in frontline roles, it jumped up to 37% that felt they were not heard.
Most providers (75%) did feel their jobs are secure. Also, unlike in the beginning of the pandemic when PPE was often hard to find, today 75% reported they have adequate PPE.
Providers' opinions of employer’s COVID-19 response
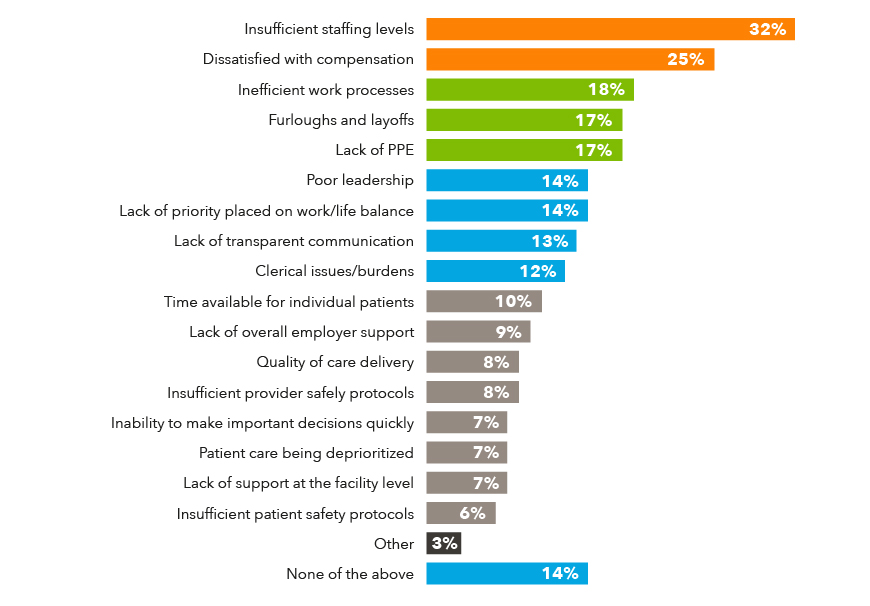
When asked about their concerns with their employer’s COVID-19 response, insufficient staffing levels (32%) followed by dissatisfaction with compensation (25%) were the at the top of the list. Inefficient work processes (18%), furloughs and layoffs (17%), and lack of PPE (17%) were also top concerns. However, 14% indicated they had no concerns with their employer’s response.
Concerns regarding employer’s COVID-19 response
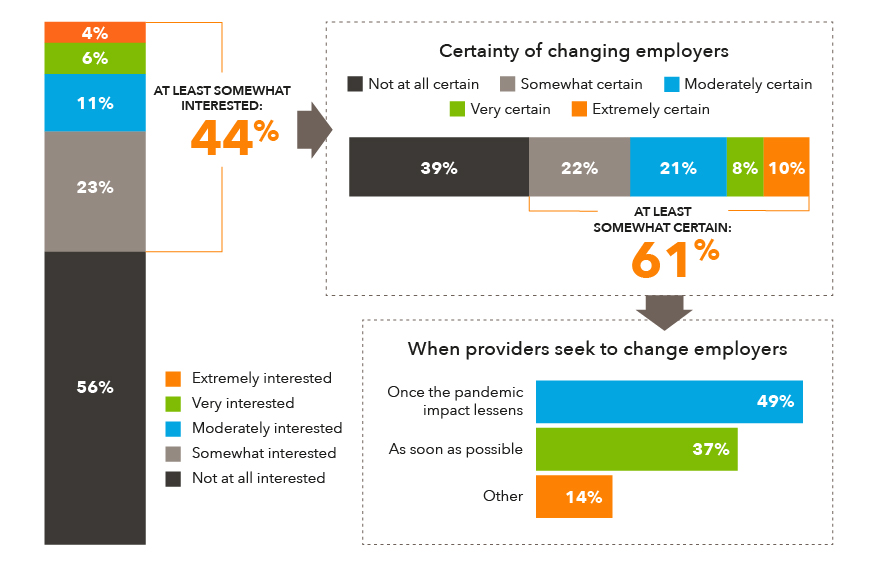
While many providers (56%) plan on sticking with their current employer, the other 44% are at least somewhat interested in changing jobs due to their employer’s COVID-19 response.
Interest in changing employers
Influences on career plans
There are a wide variety of factors that impact how healthcare providers make career decisions. The addition of COVID-19 has impacted the importance of some of those career aspects for some providers.
The most important thing providers were looking for in their careers were work/life balance (83%), job stability (78%), and workplace culture (76%).
Influential factors on provider career plans/decisions
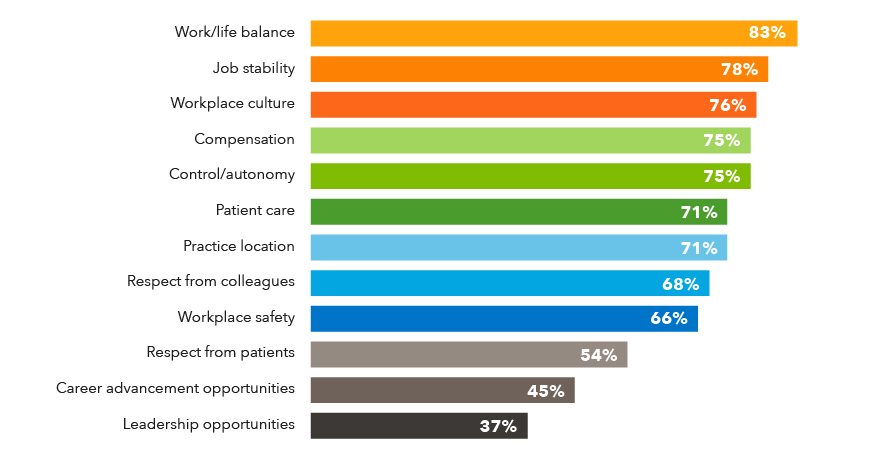
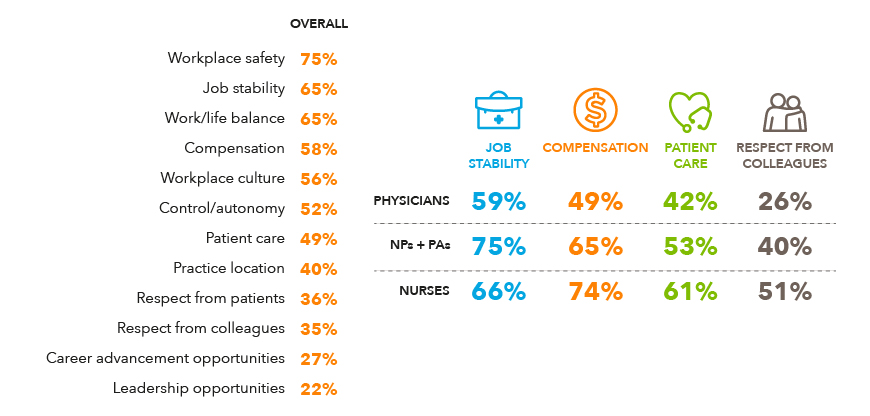
The survey also asked how those aspects of a providers’ careers were impacted by COVID-19. Not surprisingly, workplace safety was the most impacted (75%) along with job stability (65%), work/life balance (65%) and compensation (58%).
Four areas showed more dramatic differences between physicians, NPs/PAs, and nurses. Those were compensation, job stability, patient care, and respect from colleagues. For physicians, only 49% felt COVID-19 impacted their compensation compared to 65% of NPs/PAs and 74% of nurses.
For NPs/PAs, it was their job stability that was impacted (75%) compared to physicians (59%) and nurses (66%). Patient care was another area with differing opinions, 61% of nurses felt patient care was impacted by COVID-19 compared to just 42% of physicians and 53% of NPs/PAs. Finally, only 26% of physicians felt their respect from colleagues was impacted compared to 40% of NPs/PAs and 51% of nurses.
Impact of COVID-19 on aspects of provider careers
Impact of the COVID-19 vaccine on provider career plans
The COVID-19 vaccines currently being administered throughout the country have had a positive impact on providers' career plans. Three-quarters of providers (75%) had already received at least one dose of the vaccine at the time of data collection (between January and February of this year).
Impact of the COVID-19 vaccine on career plans
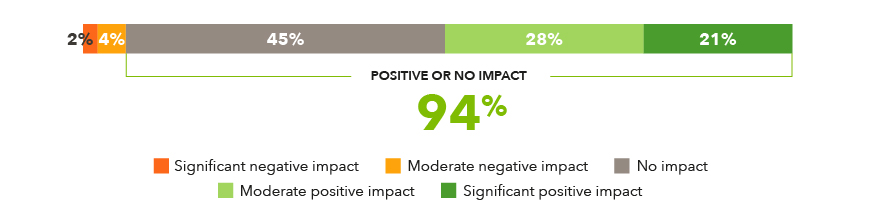
Of the 25% of providers who had not yet received the vaccine, some say they will get it as soon as possible (43%), while others plan to wait until more data is available (31%). However, about a quarter either refuse to receive a vaccine (16%) or resist doing so unless required by their employer (11%).
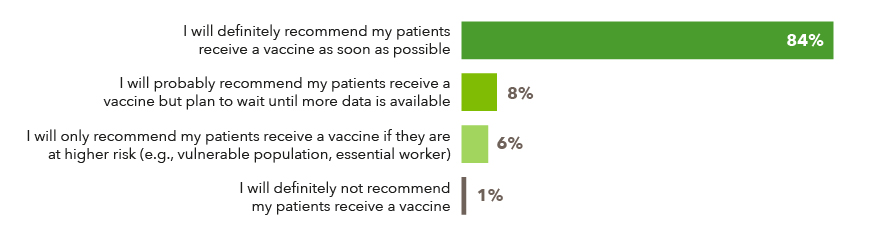
Most providers will recommend their patients receive a vaccine as soon as possible (84%).
Provider intentions to recommend vaccine
Providers still plan to work in healthcare
Even with the drop in career satisfaction and increased burnout caused by COVID-19, the survey found most providers are planning to continue working in healthcare, with just 5% indicating it is unlikely they would continue in the field.
Impact of COVID-19 on likelihood to continue in healthcare
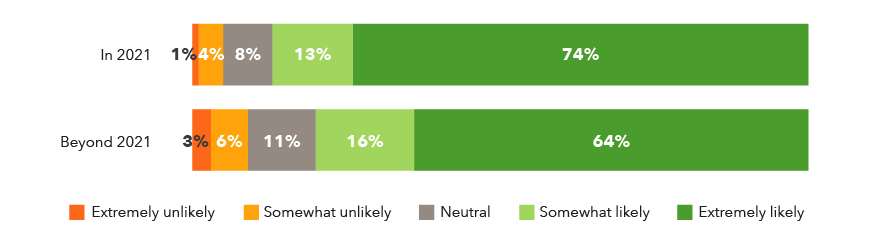
Additionally, the survey found most providers are planning to continue working in their current roles. However, those that indicated they were unlikely to stay in their current roles jumped from 13% to 24% when asked if they would continue in their current roles beyond this year.
Impact of COVID-19 on likelihood to continue in current job
Methodology
CHG Healthcare administered the survey in January and February 2021 and received responses from 1,246 individuals (623 physicians, 427 PAs/NPs, 196 nurses) across the country. The goal of the survey was to find out the views of healthcare providers on the impact COVID-19 has had on their career plans and the future expectations on the use of telemedicine.
About CHG Healthcare
CHG Healthcare is a leader in healthcare staffing. Through its family of brands, including CompHealth, Weatherby Healthcare, Global Medical Staffing, RNnetwork, Foundation Medical Staffing, LocumsMart, and Modio, CHG serves thousands of healthcare facilities and their patients around the country and the world.